Ghent - Patient participation
The empowerment of patients and caregivers is a central part of the mission at the Maria Middelares General Hospital. A positive patient experience arises from empowerment and participation. Implementation of self-control, with assured continuity of care, contributes to high-quality and patient-centered care.
Empowerment literally means that capacities are made stronger, which puts the patient and caregiver in a place to act as a the manager of his or her own care.
Empowerment assumes that people have the ability to shape their life and give it meaning. It assumes one participates fully as a citizen and share a particular consideration for socially vulnerable groups. Participation and empowerment are inseparable from each other.
Patient empowerment is a multi-factor process that gives people more control over decisions that influence their health. It situates itself on the entire care path of the patient and his/her environment.
At the Maria Middelares General Hospital, we strive to empower people in various ways.
- Empowerment as a constant in support
- Application of the participation ladder
- Working together with patient organisations
- Working together with experienced experts
Empowerment as a constant in support
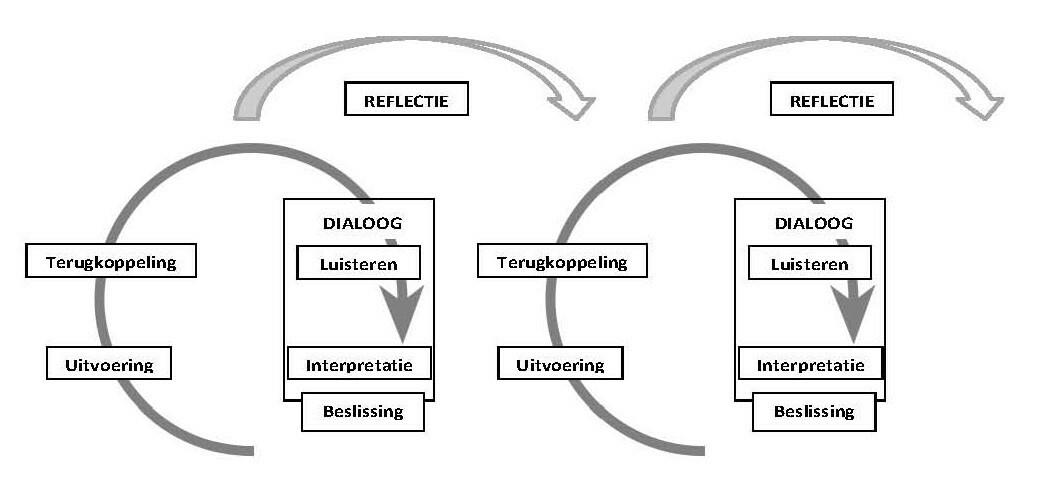
Empowerment as a constant in supportWhen providing help, we make decisions that affect someone’s life: we influence life, or even determine it at times. Participation is a process in which the decisions are shared. This process can be viewed from various perspectives. Dialogue with the patient is always the starting point. The goal is to involve the patient more in his or her treatment choices and in the outcome that is relevant for him or her. This will be done by means of appropriate, individualised tools.
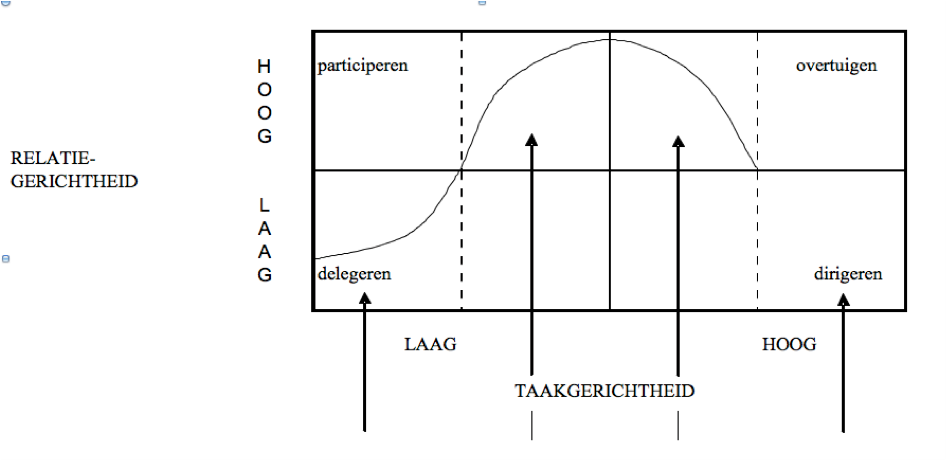
- Empowerment is a thought and treatment framework that influences our way of considering an issue as well as treating it. Participation has become an essential component in the attitude and vision of health workers. It is not so much a goal as it is a part of our way to provide high-quality, patient-centered care. Healthworkers are trained to approach patients as partners in care and treatment, and to find the right balance between dependence and independence.
- Health literacy forms an important component of this approach. We expect that everyone plays an active role and participates in care for his or her own health or disease. Even so, many people find it difficult to find the self-confidence in this process. They lack the knowledge and skills to deal with all the health information, to make appropriate choices or to take their care into their own hands. 33% (healthybelgium.be) of the Belgian population has a low health literacy. As an organisation, we take this into account with the following:
- Our website, folders, organised informational sessions, messages on social media, etc. All of these are tailored to the target audience and modified according their feedback.
- Our care professionals support people in making appropriate choices for their health by giving them the relevant information and by motivating them in this decision-making.
- At the hospital, methods that support empowerment have been used for a long time already. We strive to make the most use possible and to increase as much as possible patient competencies, and to build up a social support network for informal support, using as little professional help as possible. As a first step in guiding someone through this process, we create an overview of the patient’s abilities and needs. If we utilize all the knowledge, traits and strengths that are available, more care can be individualised and can improve one’s quality of life.
- Our health workers employ empowerment methods and strength work to help people realise what their own abilities are for managing their own existence, and to take their emotional, physical, social and material challenges into their own hands. Principles such as ‘be present’ and ‘meet the patient where the patient is at’ form the basis for this support.
- Social work has a particular focus on the most vulnerable people and offers help that can increase competencies, rights and knowledge for all patients that could then reduce social disparities in health.
- Value-based health care (VBHC) strives for shared decision making. As part of an interdisciplinary team, the care provider prepares a treatment plan of shared goals with the patient.
- In the rehabilitation care programme the ICF model is utilised. The care providers determine the treatment goals together with the patient as part of an interdisciplinary team. This model integrates the eco-bio-psycho-social model, whereby the patient is approached in a holistically. People are not reduced to their illness or vulnerability; there is consideration for the person as a whole. Our goal is to integrate this model in other care programmes, such as Geriatrics or Neurology.
Application of the participation ladder
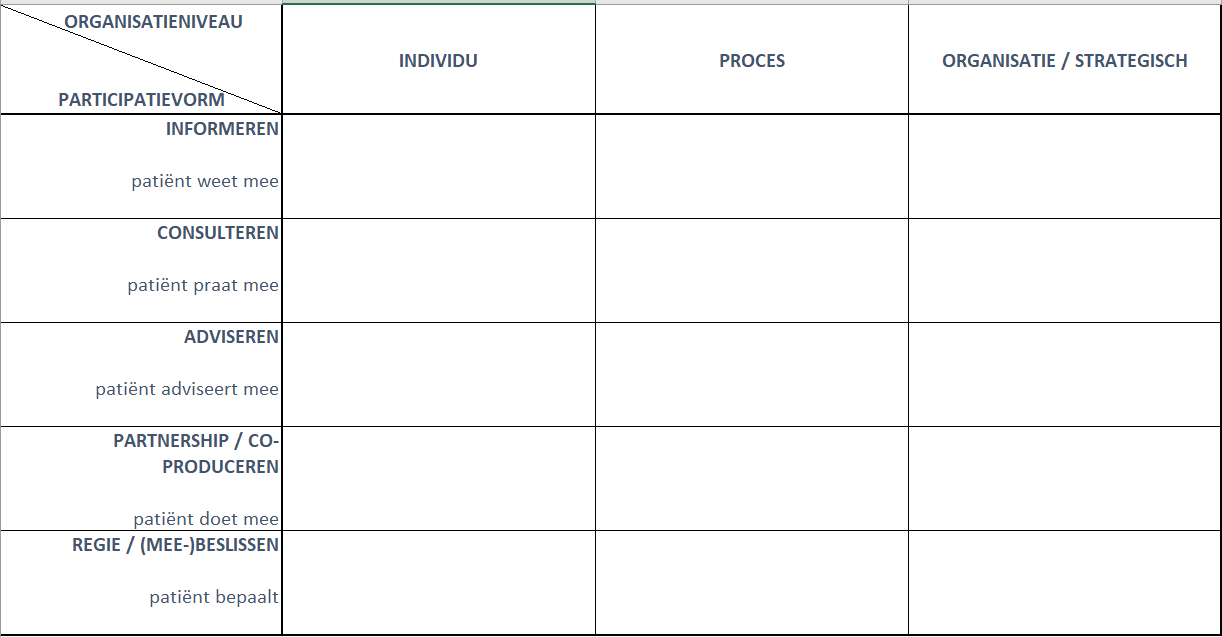
Application of the participation ladderOur goal is to use each rung of the ladder. It's not necessary for everyone or every situation to reach the highest rung on the ladder. It needs to be contextualised.
The empowerment model underlines a good working relationship and trust with the patient.
On the individual as well as the process and organisational level, we take various steps so that the patient and caregiver become more involved as a partner in the care and treatment process.
- We use oral information, folders, website, audiovisual channels and social media to educate the patient. The intention for the patient or caregiver learns along with the healthworker, taking an active role in the treatment and care process. We aim for greater trust in treatment through shared decision making and increased participation.
- There are currently various internal programmes which involve the patient or caregiver as a partner in care: Dementia and Now, Cognufiti, initiation of care planning, rehabilitation programmes, nurse office hours and oncology, etc.
- Participation increases efficacy, efficiency, and the quality of the care provided. Using VBHC, we strive to improve patient results by following up using PROMS and PREMS. Patient and caregiver experiences can then be systematically evaluated using various channels during the entire care and treatment process, during which continuity of care plays a primary role. Such evaluation informs steps for improvement in order to optimise care and treatment.
Working together with patient organisations
Working together with patient organisationsWorking with patient organisations fosters treatment compliance and patient participation. Patient organisations also improve the support and quality of care.
- We seek out collaborative, evidence-based working relationships with specific patient organisations for certain chronic pathology such as CVA, MS, coeliac disease, renal dialysis, dementia, oncology, vision problems, etc. The selection must be well thought-out, given that several patient associations may exist for the same medical condition. After making a diagnosis in the hospital, the care professional informs the patient about specific patient organisations. The patient may then voluntarily contact the organisation. In that case, the hospital provides contact person information. In this way, we work towards providing continuity of care after discharge from the hospital.
- Patient organisations we work with can request expertise in the hospital regarding study opportunities and can receive information about what we offer.
- The hospital can also make requests with the patient organisation (e.g. speaker for trainings, workshops, informational sessions, etc.).
Working together with experienced experts
Working together with experienced expertsThe patient’s contribution and experience add to joint planning that the patient and healthworkers do together. This leads to better care. Sometimes this is a matter of details, sometimes it is more a matter of the big picture.
Integration of experienced experts can bring value to the care and treatment process. Using their experience, they can increase a patient’s self-confidence. The experienced expert is complementary to the care professional. There can be several types of patients and each may participate in their care in their own particular way (patient as witness to a process, as expert after a long trajectory, as volunteer in an organisation, etc.).
- The choice of experienced expert and the integration of this expert in the team is best done with the support of an external, specialised organisation, such as Trefpunk/self-help.
- Space is created for the sick care professional to approach the patient's interests that are following their own path; the professional approaches the patient from his or her own experience, so that they can influence the care process. The advantage of this discussion is that the credibility with other healthworkers is great, even though there is the risk of a somewhat distorted picture. At the Maria Middelares General Hospital, management directly invite colleagues who are admitted to the hospital to share their experiences.
Contact
ContactDo you have a question or would you like more information? In that case, please contact Marc Vankerkhoven. This is possible Monday to Friday, 9am - 5pm.



