Hip replacement
Hip replacement
Hip replacement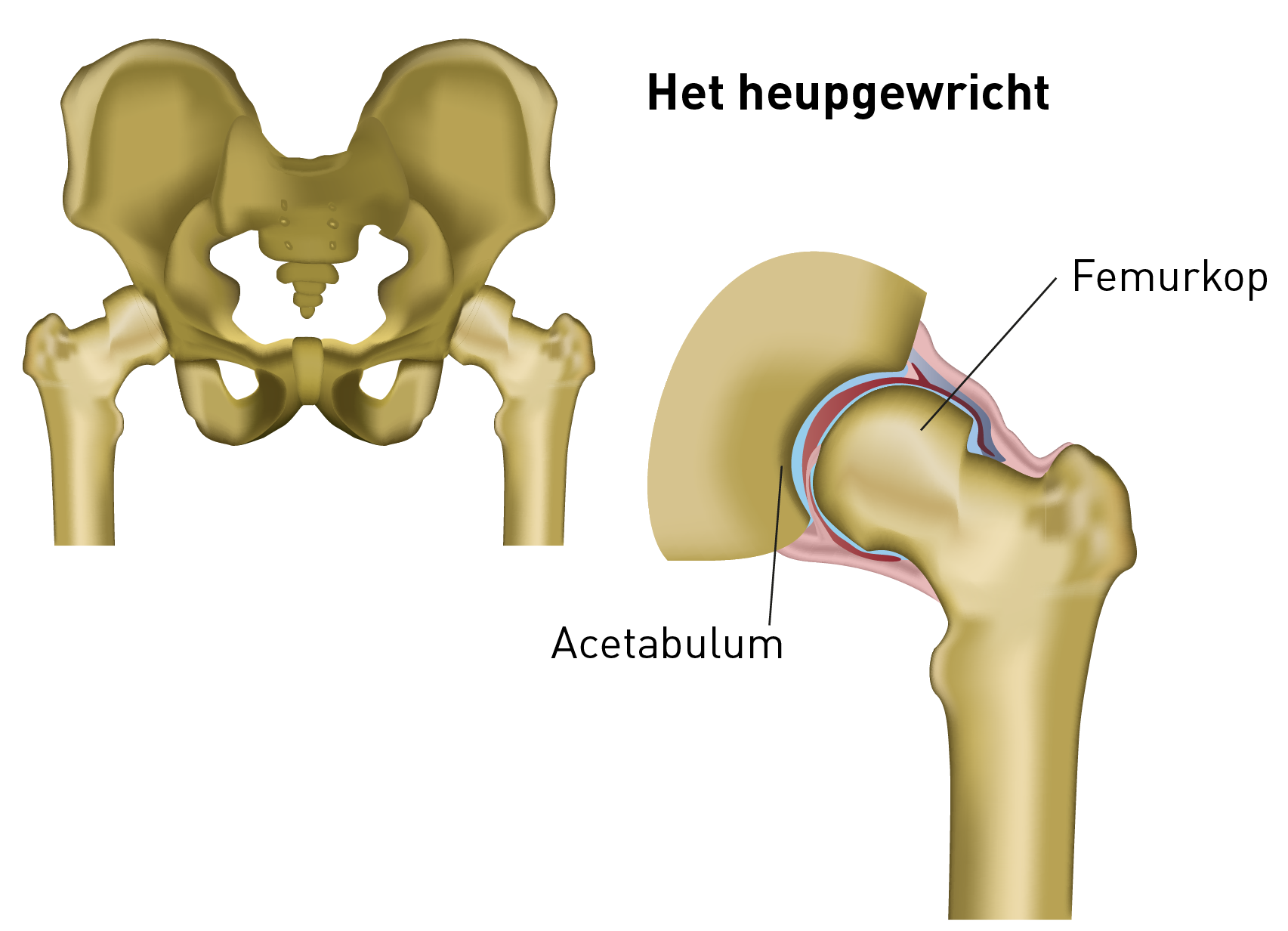
The hip joint
The hip joint consists of two parts:
- the round ball of the thigh bone (i.e. femoral head)
- the hollow socket of the pelvis (e.g. acetabulum)
When are you a candidate for a hip prosthesis?
The most common reasons for getting a hip prosthesis are:
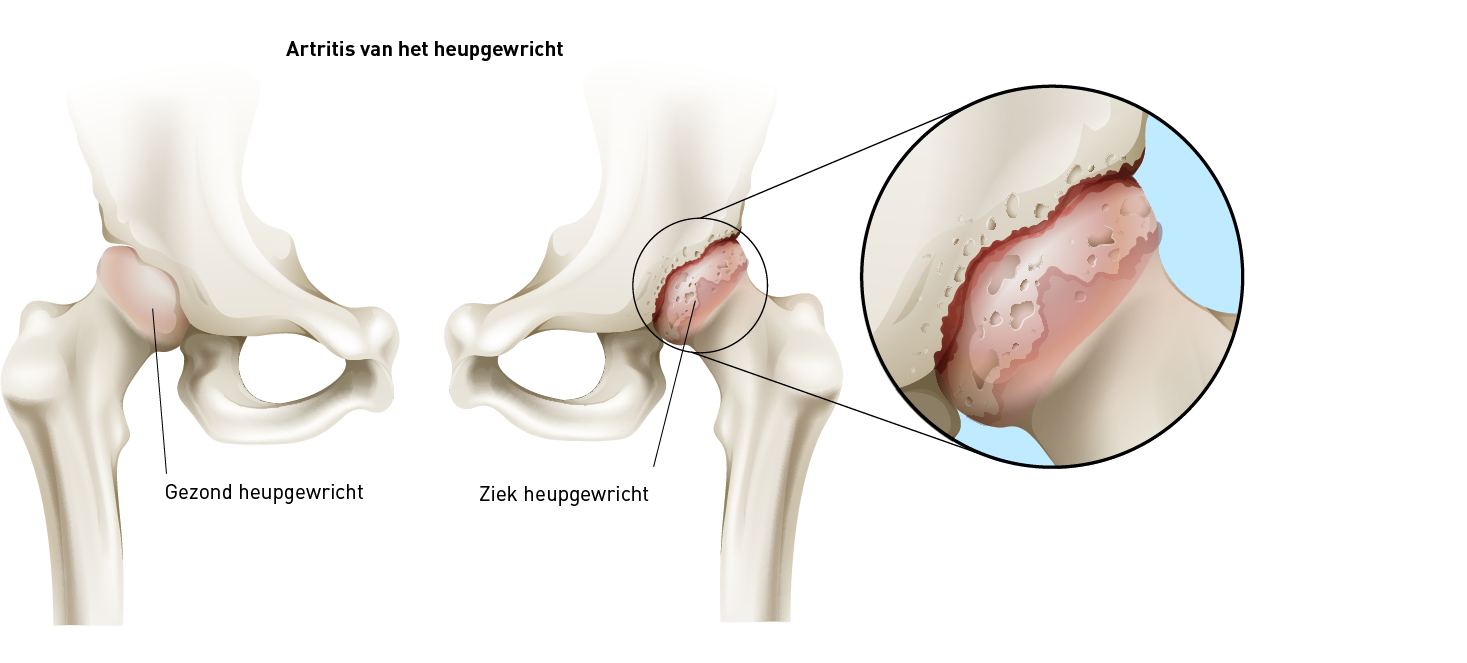
- wear and tear on the hip (arthrosis)
- hip fractures
- rheumatoid arthritis: an autoimmune disease characterised by acute and chronic inflammation of the joints and the surrounding supportive tissues
- congenital hip abnormalities: hip dysplasia
- avascular necrosis: the blood supply to the head of the thigh bone is disrupted, causing the bone to die.
Goal of the hip prosthesis
The head and the socket of a normal hip joint are covered with cartilage. If the cartilage is worn down or if there is arthrosis, each movement becomes increasingly difficult and painful.
Pain can present in the groin, the upper leg and, in some cases, can radiate to the knee. People can begin limping and some people are only able to move with the help of a cane or walker. Stiffness and difficulties with walking up and down stairs are also possible symptoms.
The goal of placing a hip prosthesis is to:
- take away the pain
- allow the hip joint to move more easily
- improve mobility and function
Total hip prosthesis
During an operation for a total hip replacement, a portion of the broken joint is removed and replaced by the prosthesis.
The way in which the hip joint is approached varies. There are three major access pathways used worldwide:
- the anterior access pathway (the front of the thigh bone)
- the lateral access pathway (from the side of the thigh bone)
- the posterior access pathway (the back of the thigh bone)
Every access pathway has its advantages and disadvantages. You may discuss these with your physician.
Poor quality cartilage and bone is shaved off in the socket and the socket portion of the prosthesis is inserted. That portion, also called the 'cup', may be completely made out of plastic (polyethylene) or a combination of metal (titanium or cobalt chrome) on the outside, with the inside made of polyethylene, ceramic or metal.
The ball of the hip is removed almost completely and replaced by a shaft that is fixated in the bone marrow canal of the thigh bone. In some cases, the exterior portion can be replaced by a shell that is placed over it (e.g. resurfacing or superficial prosthesis). The shaft is made out of metal (titanium or cobalt chrome). It can be fixed in the thigh bone with or without cement.
A ball that is the same size as the inside of the socket is placed on the shaft. The head may be made out of metal or ceramic. Discuss the selection of material as well as the advantages and disadvantages of each with your surgeon.
Possible complications
There may be complications after the procedures. Your orthopaedic surgeon will do everything possible to minimise the risk of complications.
- Bleeding: a haematoma may form around the wound sutures.
- Fever: a fever may develop a few days after the operation.
- Infection: you will be given antibiotics to prevent infection.
- Phlebitis, deep vein thrombosis and pulmonary embolism: you will receive the appropriate anticoagulant medication.
- Hip luxation or dislocation: the attending orthopaedist, physiotherapists and occupational therapists will advise you on how to keep the femoral head from coming out of the socket.
- Leg-length difference: it is possible that a small difference in leg length will be present after the operation. That different can be compensated for, if necessary, with an thicker shoe sole.
- Nerve damage: the chance of nerve damage is very small.
Several factors influence how long the prosthesis will last: being overweight and overuse can quicken the wear-and-tear process. If the hip prosthesis is worn out, it will need to be replaced. With the current prostheses and surgical techniques, the prosthesis should be able to last for 15-20 years, with normal use. It may even last you the rest of your life.
Preparation for the surgery
Preparation for the surgeryPre-operative consultation with the GP
Your GP will perform pre-operative tests. An ECG (e.g. electrocardiogram, an image of your heart) is also usually performed. Blood samples will be collected, an electrocardiogram will be performed and, if necessary, an X-ray will be taken of the lungs. In consultation with your GP, you will stop blood-thinning medications (e.g. Marevan, Plavix, Sintrom, Ticlid and Marcoumar) for at least one week prior to the surgery. Your GP will decide which medication is the best substitute.
Preparation for the discharge
Your hospital stay will be relatively brief. If you suspect that your discharge may lead to problems, we suggest that you speak with your attending physician and the hospital social worker as soon as possible, before your hospital admission. The hospital social worker will then be able to work with your
family in a timely way to look for a modified solution so that your discharge can proceed smoothly. The hospital social worker is able to provide extensive information about care and servces.
It is sometimes necessary to recuperate at a rehabilitation centre after discharge. That should be prepared for ahead of time. Besides the Prosthetic Surgery Department,
Maria Middelares General Hospital has a Rehabilitation Department, where you can go if you need more time for rehabilitation. You may contact the hospital social worker using the general phone number for Maria Middelares General Hospital: +32 (0)9 246 46 46.
Admission
AdmissionWhat should you bring to the hospital?
- Test results that you have (X-rays, ECG, blood tests).
- Crutches (you may rent these from one of the rental services through your health insurance or from a home health-care organisation).
- Closed-toe, well-fitting shoes with a wide heel that give good support and plenty of room. Keep in mind that your leg or foot may be swollen for a while after the surgery.
- Current medication list
- Home medications, in their original packaging
- Your identification card and blood type card
- (Sleeping) attire and toiletries
- long-handled shoe horn
- Please leave valuables at home
- Forms for your hospitalisation insurance
- Forms for work disability
Day of admission
On the day of admission, please arrive at the time you were given and go to the check-in desk at Maria Middelares General Hospital.
You will be given a identification bracelet to wear during your stay. Registration staff will accompany you to the care ward for Prosthetic Surgery D501. A nurse will then take you to your room. He or she will also give you the necessary information regarding your stay and will go through an intake questionnaire with you. Please shave the surgical site the day before your admission.
Please arrive at the hospital fasting. This means that you may not eat, drink or smoke after the time indicated by your physician. He or she will also tell you which daily medications to take on the day of your admission. Smoking not only negatively affects your breathing during anaesthesia, but it can also negatively affect the prosthetic bone growth afterwards. Smoking is also prohibited in the hospital.
It is also important to remove your contact lenses or glasses, dentures, hearing aids, nail polish, make-up and piercings before the operation.
If the department nurse gets a call saying that the OR is ready for you, he or she will let you know and help you put on the surgical gown.
The operation
The orthopaedic surgeon and the anaesthesiologist will come see you before you undergo anaesthesia. Please make sure to ask any questions you may have about the anaesthesia or the operation.
The total hip operation lasts for approximately one hour and is performed while you are under anaesthesia. There are two types of anaesthesia: general anaesthesia and local anaesthesia (spinal block).
The time spent in pre-operative preparation, the operation itself and the recovery room can lasts up to four hours. If you are completely awake, the pain is under control and your vital signs are normal (blood pressure, pulse, respiratory rate, pain scale, etcetera), you will be brought back to the care ward.
After the operation, you will receive:
- An infusion: a thin, flexible tube will be inserted into a blood vessel to administer fluids, pain medication and antibiotics.
- A nasal cannula is sometimes necessary to administer oxygen.
- A Redonis sometimes necessary: a catheter that is placed in the wound to drain tissue, fluid and blood.
- A leg support cushion: on the operated leg, in order to prevent the weakened leg muscles from turning your leg sideways, causing your hip to dislocate. The nurse will turn you appropriately, onto your non-surgical side, during post-surgical care.


Pain scale
After the operation, the medical and surgical team will do everything they can to treat your pain. The pain will be recorded on our care ward. This allows us to gain better insight into the intensity of your pain. Explaining how much pain you have is not always an obvious task. Rating it with a number between 0 and 10 can help us understand how much pain you are experiencing. In the department, a visual pain scale is used where 0 is no pain and 10 is severe pain.
Post-operative care and recovery
The day of the operation
When you come back to the care ward, you may drink and eat (a light and easily digestible lunch) as soon as you are able. You may be nauseous or need to vomit. The nurse will give you medication for those symptoms, if necessary. Your home medications can be restarted as per the advice of your physician.
You may not take any sleep medication on the day of operation. Your bandage and vital signs will be checked and recorded every four hours during the first twelve hours. You will be regularly offered an ice pack to place on the surgical site. That helps alleviate the pain and to minimise swelling.
The following day
The day after the operation, the IV and Redon, if placed, will be removed.
The nurse will help you with going to the toilet in the morning and will help you out of bed. Your bandage will be checked daily. It will be replaced only if it is completed soaked through (with drainage from the wound or blood). During your stay, the occupational therapist and physiotherapist will meet with you daily (except Sundays) to complete a rehabilitation programme and to achieve the following concrete goals:
- to be able to move around independently, such as in and out of bed, to the toilet, etcetera
- to take steps correctly and safely using a walker or crutches
- to walk up and down stairs safely
Exercises are necessary for a good recovery and to regain the mobility and strength in your hip. The physiotherapist and occupational therapist will start the rehabilitation in the hospital and you will be given exercise instructions and recommendations for how to do them at home.
Discharge
DischargeYou will be ready to go home any time after two days or up to one week after the operation. This will depend on the nature of the procedure, wound healing, your general recovery and the rehabilitation. Some people, however, will temporarily stay on a Rehabilitation Department.
On the day of discharge (depending on the attending physician), your wound sutures will be taken care of and the bandage will be replaced. You may shower with the bandage on but may not take a bath. If the bandage is dry and not coming loose, leave it on until you see your GP to have the sutures or staples removed. If your wound is still moist, you may be prescribed wound care at home.
Every patient will have X-rays taken of the hip (follow-up image). This may also be carried out at your discharge.
At the time of discharge, you will be given the following documents:
- a discharge letter for your GP, depending on the attending orthopaedist
- a prescription for home nursing care (if necessary)
- a prescription for medication
- an appointment or invitation for the first follow-up check/consultation, approximately six week after the procedure
- a prescription for follow-up physical therapy
- a medication list
Contact the attending orthopaedist if one or more of the following symptoms occur:
- sudden increase, pain intolerability
- fever
- draining wound more than ten days after the operation
- redness, pain and warmth where the wound sutures are placed
- shortness of breath
- pain in the calf
- purulent and foul-smelling drainage from the wound sutures
Tips for at home
Tips for at home- To get dressed, it is best to start with the leg that was operated on. To get undressed, start with the non-surgical leg.
- Listen to your body. Pain or discomfort mean that it is better to do things a bit more slowly.
- During the first couple of months after the operation, it is recommended that you not bend forward deeply, cross your legs, do heavy lifting nor stand up directly from a sitting position in a deep chair.
- You can find information about medical aids in the Home Care shop. These can help make life at home easier and more comfortable with aids such as an elevated toilet seat or a hospital bed.
- You need to have difficult infections (e.g. urinary tract infections, lung, skin or dental infections) treated immediately. Consult your physician if you have any of these, especially if you have a fever.
- It is best to not receive any injections in the site of the hip operation.
The contents of this website are only meant to serve as a guideline. The goal of this website is to inform you as much as possible about how an artificial hip is placed. Even so, you may have questions. Please do not hesitate to contact our nurses at the care ward or to contact your attending orthopaedist.
Only available in Dutch:
Brochure heupprothese
DownloadCost estimate
Cost estimateCentres and specialist areas
Centres and specialist areasLatest publication date: 16/01/2024




