Hiatal hernia
Symptoms and causes
Symptoms and causesWhat is it?
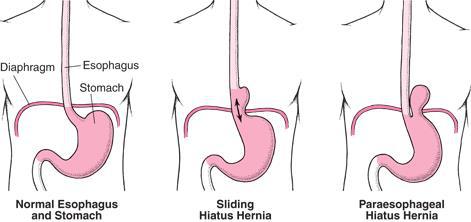
The diaphragm (the muscle that separates the thoracic cavity from the abdominal cavity) has an opening through which the oesophagus proceeds from the chest to the abdominal cavity. A diaphragmatic hernia occurs when this opening is wider than necessary.
The transition from the oesophagus to the stomach is exactly where the oesophagus passes through the diaphragm. There, the oesophagus makes an acute angle (angle of His). This angle becomes sharper when the stomach is filled (when eating) and the diaphragm contracts. This angle then acts as a kind of valve and prevents stomach contents from flowing back into the oesophagus.
If the opening of the diaphragm is too wide, the natural 'angular position' between the stomach and oesophagus is disturbed. Consequently, the stomach contents can flow back into the oesophagus more easily. This occurs quicker and more strongly when the patient lies flat on the back or bends forward, Because gravity no longer helps keep the acid in the stomach.
The terms abdominal rupture, hiatal hernia, diaphragmatic hernia and sliding hernia are usually used interchangeably, but they actually have different meanings.
When the transition from the oesophagus to the stomach is located in the thoracic cavity, instead of the abdominal cavity, it is called a ‘sliding hernia’ (see image).
A diaphragmatic hernia may be present at birth. As a result, even the small intestine, colon or spleen can enter the thoracic cavity.
When the hernia occurs later in life, it is usually due to slackening of the diaphragm. This could be due to old age or, in rare cases, an accident (with a tear of the diaphragm).
A major risk factor for developing a diaphragmatic hernia is increased pressure in the abdomen due to a greater amount of fatty tissue in the abdomen, chronic coughing, hard pressing during bowel movements, pregnancy...
Symptoms
A diaphragmatic hernia in itself does not cause any symptoms. The hernia is usually discovered by accident.
Typical reflux symptoms of reflux include:
- acid regurgitation
- nagging/burning pain behind the sternum
- swallowing problems
- when the gastric acid reaches the throat or mouth, it can cause local irritation, foul-smelling breath and tooth erosion
- hoarseness (because of its impact on the vocal cords), cough or asthma (because of its impact on the airways) may also occur
- if the reflux of gastric acid to the oesophagus is prolonged and regular, the oesophagus can become irritated and inflamed (reflux oesophagitis), sometimes resulting in blood loss or constriction (stenosis).
- during prolonged exposure, the mucous membrane of the oesophagus may gradually change (Barrett’soesophagus), which increases a person’s risk of developing adenocarcinoma (cancer) of the oesophagus.
- persistent reflux symptoms can lead to a lower quality of life due to poor sleep (reflux becomes worse when you lie down flat) or because certain activities cannot be performed because yow cannot bend over.
Diagnosis and treatment
Diagnosis and treatmentHow is it diagnosed?
- pH-metry
- gastroscopy
- manometry
- X-MSD: during a contrast swallow (X-SMD or oesophagus-stomach-duodenum examination), the patient drinks contrast medium under X-ray. This will visualise the transition from the oesophagus to the stomach. It ensures a diaphragmatic hernia can be identified. It also shows the specific size. In addition, problems relating to the passage through or the reflux of the contrast fluid in the oesophagus can also be identified. Finally, the length of the oesophagus can be measured, which is important if surgical treatment is considered.
Treatment
Read more about the different treatments: Hiatus hernia repair
Treatment centres and specialisations
Treatment centres and specialisationsLatest publication date: 15/05/2024



