Sentinel lymph node removal
What is it?
What is it?Two treatments of the armpit are possible: removal of the sentinel lymph node and removal of all lymph nodes from the armpit.
Surgery for breast cancer not only involves the removal of the tumour, but also of the armpit lymph nodes. This is because there is a chance that underarm lymph nodes are already affected by the tumour.
The lymphatic vessels of the chest and the arm come together in the underarm lymph nodes. This is where the lymph is filtered. When breast cancer spreads (metastasises), it spreads to the lymph nodes in the armpit first in the majority of cases. Therefore, the lymph nodes also function as a first filter for the metastasising breast cancer cells, with the purpose of stopping them. The larger the tumour or the more aggressive, the greater the chance of metastases in the underarm nodes. It is important to remove these nodes, on the one hand to stop these affected glands from growing and forming large tumours in the armpit, and on the other hand to find out whether the lymph nodes have been affected. The latter has an important predictive significance and will often be the reason to administer additional treatment (chemotherapy, radiotherapy of the armpit).
Because until a few years ago it was impossible to know which lymph nodes were connected to the breast and which ones were not, as many lymph nodes as possible were removed (sometimes more than 20). This is called axillary lymph node dissection. It involves the removal of all lymph nodes that drain lymph from the breast. The lymph nodes are embedded in fatty tissue that is removed in its entirety. The important nerves and blood vessels are spared. Removing the underarm fat results in a cavity. After the wound is closed, a vacuum drain is used to drain superfluous wound exudate (blood and lymph). Sometimes, this drain needs to remain in place for a few days.
Since, often, none of these glands turned out to be affected and because axillary lymph node clearance frequently lead to discomfort such as lymphoedema (fluid accumulation) of the arm, surgeons sought a way to remove the underarm lymph nodes in a more selective manner. To that end, a new technique was devised: the sentinel lymph node removal.
What does a sentinel lymph node removal constitute?
What does a sentinel lymph node removal constitute?The sentinel lymph node is the first lymph node that is directly connected with the tumour through a lymphatic vessel. Tumour cells can spread to the other glands from the sentinel lymph node. If the sentinel lymph node is found to be normal, no further underarm surgery is required. However, if the sentinel lymph node contains breast cancer cells, the other lymph nodes must be removed too. This sentinel lymph node removal applies to small breast cancer abnormalities. In the case of larger tumours, or if multiple tumours are present in one breast, the classic axillary lymph node clearance is still opted for.
Procedure
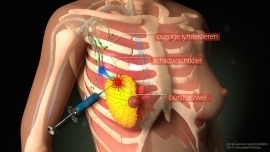
ProcedureBefore the procedure, the physician injects a radioactively marked substance (tracer) into or near the tumour. The product flows to the lymph nodes through the lymphatic vessels in the same way as tumour cells. Imaging (scintigraphy) can visualise the sentinel lymph node(s). The physician will mark the skin using a coloured marker at the location of the sentinel lymph node.
During the procedure, the surgeon uses a special device (a gamma probe) to find and remove the radioactive gland(s).
Sometimes, a blue dye is injected into the breast with the same purpose, that is to detect the first draining gland(s). In some cases, one single sentinel lymph node is involved, but often there are two or more such sentinel nodes. The sentinel lymph node removal procedure can save a great many patients from a full axillary lymph node clearance procedure. If the procedure is scheduled late in the morning or in the afternoon, the tracer is injected the morning of the same day. If the procedure is scheduled for the early morning, the tracer is injected in the late afternoon of the preceding day.
Centres and specialist areas
Centres and specialist areas
Latest publication date: 16/05/2024
Supervising author: Dr Elzo Kraemer Ximena






