Gastroscopy
What is it?
What is it?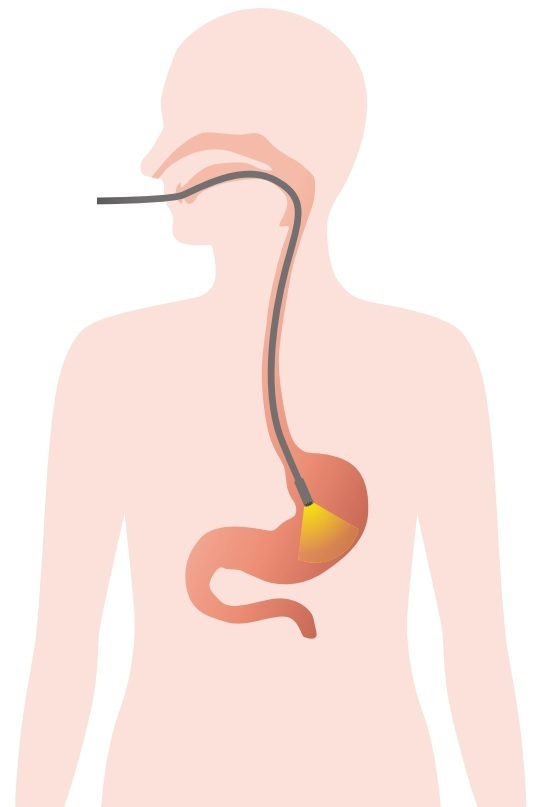
A gastroscopy is the most accurate and sophisticated examination available for the oesophagus, stomach and duodenum. During the examination, a flexible tube with a video camera is inserted through the mouth. Th examination can detect inflammation, ulcers, polyps and many other conditions at an early stage.
Other examinations for gastrointestinal symptoms are:
However, these do not provide the same accurate information.
If your physician recommends a gastroscopy and you decline, that may result in a delayed or mistaken diagnosis, with possible unpleasant consequences and therapy options that are not optimal.
Things to consider
Inform us if:
- pregnancy
- allergy, sensitivity or intolerance (e.g. latex, Lidocaine)
- clotting problems or use of blood thinners (e.g. Marevan, Sintrom, Marcoumar, Ticlid, Plavix, Pradaxa, Xarelto, Aspirin)
- artificial valve or prosthetic: some patients require antibiotics before and after the procedure;
- epilepsy, diabetes, chronic heart, lung and kidney disorders: special attention to medication required.
Do not hesitate to ask for additional explanation should you have any doubts or queries.
Course of the procedure
Course of the procedurePreparation
- You must fast for at least six hours before the examination. If the examination is performed in the afternoon, you may take a light breakfast (sandwich with jam or cheese spread).
- Do not smoke on the day of the procedure, and smoke as little as possible in the preceding days.
- Dental prostheses are best removed in advance. Damage to teeth (higher risk if teeth are in poor condition) cannot be ruled out during an endoscopy or anaesthesia.
Examination procedure under local anaesthetic
This examination can be done under light local anaesthetic with a Xylocaine throat spray. You will be conscious during the examination.
Upon arriving at the hospital, you can sign in at the e-kiosk with your ID card.
- Maria Middelares General Hospital: in the atrium
- St Vincent General Hospital in Deinze: at the A&E entrance (Meulenstraat)
- Medical centre in Ghent-Bruges: in the entrance hall
After registration, you will be directed to the waiting room where the nurse will come to collect you:
- Maria Middelares General Hospital: waiting room A1.03 (first floor)
- St Vincent General Hospital in Deinze: route 77 (third floor)
- Medical centre in Ghent-Bruges: waiting room 36 (first floor)
After the examination, you may experience mild throat irritation. You are allowed to drive yourself home.
Examination procedure under general anaesthesia
Anxious patients or patients who must undergo the examination repeatedly (e.g. to treat oesophageal varices or for stretching of a narrowed oesophagus), may opt to have the examination done under general anaesthesia.
A gastroscopy under general anaesthesia can be scheduled at Maria Middelares General Hospital or St Vincent General Hospital in Deinze. This is performed on an outpatient admission basis. For a preliminary consultation before the examination, you can make an appointment.
Ask for specific guidelines if you have diabetes, epilepsy, chronic heart, lung or kidney disorders or if you take blood thinners.
If you opt for a general anaesthetic, an intravenous drip will be placed in a vein of your arm to deliver the medication. After general anaesthesia, you wake up in the recovery room or the short-stay room. You may experience mild throat irritation, mild drowsiness or dizziness (due to anaesthesia) after waking up.
Afterwards, you will not be allowed to drive yourself home and will be unable to work for the rest of the day. Do not plan any important activities after the procedure. Your concentration and judgement may be diminished.
Safety and hygiene
We are an experienced and well-trained team, equipped with a modern infrastructure.
If you have opted for anaesthesia, an anesthesiologist will be responsible for this.
The procedure is performed in an endoscopy room that is equipped with all the necessary anaesthesia equipment and endoscopy instruments. Before and after each test, each endoscope is thoroughly cleaned and disinfected in an automatic cleaning and disinfection machine in a controlled procedure. Our disinfection protocols meet European standards. We use disposable materials for taking tissue samples (biopsy), injecting medication and removing polyps.
Potential risks
Potential risksIn principle, complications hardly ever occur.
- A very rare complication is perforation (i.e. tear) of the stomach or oesophagus. In that case, you will need urgent surgery.
- Stretching of narrowed parts (balloon dilation of stenosis), the treatment of varicose veins (i.e. varices) and the stemming bleeds rarely result in perforation complications.
- Bleeding as a result of gastroscopy is rare and can usually be treated without the need for surgery.
- In rare cases, phlebitis can develop at the IV insertion site.
Contact us if you have the following symptoms after the procedure:
- persistent severe pain
- fever
- blood loss (red or black stools)
- any concerning symptom
Cost estimate
Cost estimateCentres and specialist areas
Centres and specialist areas
Latest publication date: 16/05/2024
Supervising author: Dr Monsaert Els




