Liver fibrosis and cirrhosis
Symptoms and causes
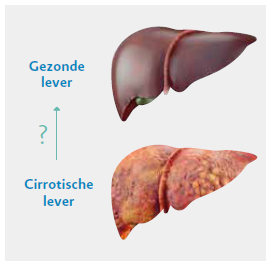
Symptoms and causesChronic liver diseases are accompanied by constant inflammation of the liver, also known as hepatitis . Chronic inflammation causes liver lesions (i.e. damaged liver cells). During the healing process, fibrotic tissue provides a basis for closing the wound. As the disease progresses, liver fibrosis increases. This is measured by the Metavir score, which ranges from stage F0 (no liver fibrosis) to F4 (liver cirrhosis). Stage F4 is also called liver cirrhosis, the final stage of progressive liver fibrosis. Regenerative nodules and an altered structure of the liver tissue are characteristics of liver cirrhosis [1-3].
Metavir. A scoring system based on the histopathological assessment of a liver biopsy to evaluate the degree of inflammation (A0-A3) and the fibrotic stage (F0-F4). Metavir stages F0-F1 correspond to mild liver damage, metavir stage F2 to significant liver fibrosis of the portal fields and metavir stages F3-F4 to advanced liver fibrosis, pre-liver cirrhosis or liver cirrhosis.
Liver cirrhosis is a spectrum with two stages: compensated and decompensated liver cirrhosis. The compensated condition corresponds to Child-Pugh score A, while the decompensated liver cirrhosis corresponds to Child-Pugh score B (moderate) or C (severe). In patients who have compensated liver cirrhosis, the liver is still functioning, whereas in patients who have decompensated liver cirrhosis the liver function is severely impaired. Characteristics of decompensation are ascites, varicose veins in the oesophagus, jaundice, hepatic encephalopathy, etcetera. These patients are highly vulnerable. Removing the harmful influence reduces the risk of further decompensation.
Child-Pugh score. A score that is used to make a prognosis of chronic liver diseases (especially liver cirrhosis) and to estimate the progression of liver cirrhosis. The score lies between 5 and 15 and is based on five parameters: albumin and bilirubin values, prothrombin time, ascites and hepatic encephalopathy. Patients who have 5 or 6 points obtain a Child-Pugh score of A. This means that they have compensated liver cirrhosis but that the liver is still functioning well. Scores of 7-9 points and >9 points indicate decompensated liver cirrhosis and correspond to Child-Pugh score B and Child-Pugh score C, respectively.
Live cirrhosis can reduce life expectancy and make the patient more susceptible to several complications. If the liver becomes further damaged, liver cirrhosis evolves from a compensated to a decompensated form, and the patient has symptoms of severe liver failure: portal hypertension with bleeding varicose veins, encephalopathy, jaundice or ascites.
However, cirrhosis of the liver is not reversible and the patient must, for example, be checked every six months for early detection of liver cancer . Treatment of decompensated patients must be looked at on a patient-by-patient basis. Often the consequences of terminal liver disease such as ascites, varicose veins and/or hepatic encephalopathy are disastrous for the patient's quality of life.
Sources
- Bedossa P. et al, Hepatology 1994; 20(1 Pt1): 15-20.
- Poynard T. et al, BMC Gastroenterology 2010, 10: 40.
- Sebastiani G. et al, World J Gastroenterol. 2014, 20(32):11033-53.
A few terms
- Ascites: fluid accumulation in the abdominal cavity. A terminal liver disease in combination with portal hypertension can lead to the development of ascites.
- Portal hypertension: elevated blood pressure (>12 mm Hg) in the portal vein. The main cause of portal hypertension is an obstruction of the blood circulation in the liver, such as nodules in liver cirrhosis. This condition can have serious consequences, such as ascites, oesophageal varices and haemorrhoids.
- Hepatic encephalopathy: neuropsychiatric disorders in patients who have liver failure, often characterised by cognitive (mental) problems, confusion and a changed level of consciousness.
- Oesophageal varices: enlarged and abnormally swollen veins in the oesophagus. They lead to a permanent and pathological change of the vessel walls. Usually, they are the result of the portal hypertension caused by cirrhosis. In an attempt to compensate for the blood supply to the liver, the blood flows to smaller vessels, which may leak and rupture. This can cause life-threatening bleeding.
Diagnosis and treatment
Diagnosis and treatmentPatients who have cirrhosis are known to have an increased risk for primary liver cancer. Chronic liver damage can cause the liver cells to become malignant. Unfortunately, such patients can only heal if liver cancer is discovered at an early stage. It is therefore of paramount importance that patients who have cirrhosis are regularly checked for liver cancer. It is advisable to have an ultrasound every six months so that lesions can be detected and treated as quickly as possible. Currently, we cannot prevent liver cancer. That is why it is very important to treat patients before they develop cirrhosis. Moreover, we should realise that treatment can prevent further progression of liver fibrosis and liver decompensation. Patients who have already developed cirrhosis are still at risk have a of getting liver cancer. That is why patients with liver cirrhosis must be examined every six months.
Is liver cirrhosis reversible?
In some cases, liver cirrhosis is partially reversible. However, there is as yet no evidence of a complete cure for liver cirrhosis (i.e. a return to the normal liver structure).
Source:
- Povero D. et al, Histol Histopathol. 2010;25(8):1075-91.
Which factors can influence the progression of liver fibrosis?
Genetic factors may play a role in the progression of liver fibrosis, but there are also other factors, such as alcohol consumption, the viral infection that caused the liver disease, diabetes mellitus and the patient's age, gender and weight. In patients with hepatitis C, the progression of liver fibrosis is strongly influenced by age, alcohol consumption and male gender.
Sources
- Poynard T. et al, Lancet 2003;362(9401): 2095-100.
- Poynard T. and Afdhal, N., AntiVir Ther 2010;15(3): 281-91.
- Poynard T. et al. Lancet 1997; 349(9055): 825-32.
Do I have to follow a special diet if I have a chronic liver disease?
It is advisable not to drink alcohol and to follow a balanced diet, especially for patients suffering from gall bladder problems and gallstones. Be sure to ask your physician for advice on a healthy diet.

Treatment centres and specialisations
Treatment centres and specialisations
Latest publication date: 15/05/2024
Supervising author: Dr Monsaert Els



