Liver disease, alcoholic
Symptoms and causes
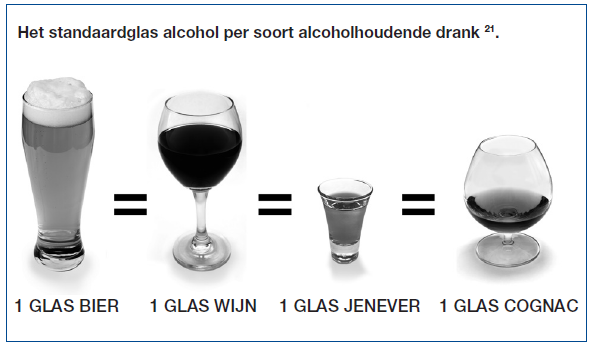
Symptoms and causesWhen we talk about alcohol consumption, we express it in terms of drinks. An alcoholic beverage contains approximately ten grams of pure alcohol, regardless of the type of drink. Two glasses of wine - consumed for example at mealtimes - contain 20 grams of alcohol. This is based on the average catering size. Of course, the question immediately arises as to how much alcohol consumption could cause liver disease. Research has shown that both the quantity and duration of use determine the nature and severity of liver damage. We now also know that there are hereditary factors that help determine whether or not there will be liver disease.
Even with relatively low alcohol consumption, women are more likely to get liver damage than men. In addition, liver disease seems to develop more rapidly in women.
Liver abnormalities often remain unnoticed for a long time and only come to light when actual liver cirrhosis (shrinkage of the liver) occurs. Mortality from alcoholic liver cirrhosis in the western world is now estimated at around three million people a year! This makes alcoholic liver disease one of the most common liver diseases in our part of the world.
Detrimental effects of alcohol
Alcohol cannot be stored and must therefore be broken down immediately in the body. The break-down takes place in the liver and is made possible by the enzymes. Excessive alcohol supply can lead to metabolic disorders due to the accumulation degradation products. This results, for example, in a disorder of the fatty metabolism in the liver, which is reflected, among other things, in increased triglyceride (fatty acid) content. Furthermore, metabolic disorders can cause uric acid levels to rise, possibly causing gout attacks and other problems.
The processing of alcohol differs from person to person and is partly determined by a hereditary predisposition. The question of how much alcohol can be consumed without harmful effects on the liver is therefore not so easy to answer. Because we cannot know exactly per person and there are major individual differences, we maintain a safety margin. In women, two drinks a day, in men three to four.
A choice is made among various techniques based on the type of haemorrhoids, the type of symptoms and some patient-specific characteristics:Fatty liver can often be seen on ultrasound and, of course, on a liver biopsy. By stopping alcohol consumption, steatosis quickly disappears. The liver cells do not necessarily suffer permanent damage as a result. When there is an infection, then it is different. Infection causes damage to the liver.
A clear acute hepatitis can occur after a considerable amount of excessive alcohol consumption, usually in combination with, for example, prolonged bad eating, an infection, vomiting or diarrhoea. There is usually obvious jaundice. Laboratory tests reveal significant liver function disorders and a markedly increased number of white blood cells. Furthermore, usually an enlarged, painful liver. This situation can also cause ascites (fluid accumulation in the abdomen). Alcoholic hepatitis mainly occurs in a liver that is already fatty, but also in livers that are already cirrhotic. In the latter case, of course, a more serious situation arises.
In an alcoholic liver, the fibrosis (the connective tissue) lies directly around the liver cells. This form of fibrosis compresses the space through which the blood vessels pass, thus impeding the flow of blood. As a result, high blood pressure develops early on in the blood vessels of the abdomen (portal hypertension) without cirrhosis of the liver. Liver fibrosis can be checked with an elastography measurement (e.g. fibroscan). This is a form of medical imaging using a small device that is held against your abdomen, which takes images of the liver and calculates a type of 'stiffness'. You can imagine it as a kind of ultrasound machine with additional capabilities; it is also completely painless, safe and does not emit any medical radiation. Liver cirrhosis is caused by greatly increased fibrosis, with only islands of healthy liver tissue. We call these noduli. Cirrhosis can develop unnoticed without the presence of alcoholic hepatitis. The first symptoms may be an ascites belly or a haemorrhage from oesophageal varicose veins.
In the cirrhotic liver, a primary liver cell carcinoma may develop.
Diagnosis and treatment
Diagnosis and treatmentDiagnosis
The anomalies found in laboratory tests are rarely direct evidence of alcoholic liver disease. A combination of elevated transaminases (ASAT and ALAT) with high triglyceride levels and high gamma-Gt levels may indicate alcoholic liver disease especially if uric acid levels are also elevated.
Steatosis can often be demonstrated by ultrasound examination of the abdomen. Other causes of alcoholic hepatitis should be excluded. It is often possible to draw the conclusion from past history that alcoholic hepatitis is involved. Sometimes, however, it is necessary to perform a liver biopsy. Pathological examination of a piece of liver tissue may reveal typical abnormalities indicating alcohol as the cause of the hepatitis.
Treatment
The most important and also only thorough measure in a patient who consumes too much alcohol is to stop the alcohol intake completely. If this is successful, life expectancy will improve even in the case of pre-existing liver diseases. Liver cirrhosis has only a low chance of recovery, but fibrosis and fatty liver can diminish or even disappear. In addition to stopping alcohol, adequate nutrition plays a very important role. In situations of malnutrition, which is usually the case with cirrhosis, the number of calories must be high and the diet must contain sufficient protein. Ideally, the food intake should be divided over several meals a day, including in the evening before bedtime. Special diets are rarely needed. Additional vitamins should only be used if there are deficiencies.
Treatment of alcoholic liver cirrhosis
This treatment is not specific and is aimed at treating complications such as portal hypertension, ascites and encephalopathy (alteration of the brain tissue). It is important that the dosage of medications may need to be adjusted if necessary. In the case of alcoholic cirrhosis of the liver, one should be particularly cautious with sleep-inducing medications and sedatives.
Liver transplantation in cases of alcoholic liver cirrhosis
At the end stage of liver cirrhosis, a liver transplant can also be performed in this group of patients. Since this disease is self-inflicted, the patient must meet a number of conditions. There must be a stable social situation. Furthermore, there must be no alcoholic organ damage outside the liver. In addition, the patient should not have consumed alcohol for at least six months.
If a liver transplant is performed, the results are relatively good compared to transplantats in other forms of liver cirrhosis. It is therefore now generally accepted that there are no good moral or medical reasons to exclude patients with alcoholic liver cirrhosis from a liver transplant.
Liver patient and alcohol
As previously stated, a healthy liver can process two to three glasses of alcohol a day without suffering damage. This is clearly different in the case of patients who already have liver damage for another reason. In that case, even a small quantity of alcohol can make the condition of the liver worse. Therefore, it is not good for patients with any form of hepatitis, steatosis, fibrosis or cirrhosis to consume alcohol.
Treatment centres and specialisations
Treatment centres and specialisations
Latest publication date: 15/05/2024
Supervising author: Dr Monsaert Els



